
Alumni
This person is a member of Sanger Institute Alumni.
Collectively, enteric infections and neglected tropical diseases cause an estimated two million deaths a year and 100 million years of healthy life lost. This would be equivalent to the entire population of London each losing 11 years of healthy life. Children are most affected, and indirect effects such as costs to caregivers and malnutrition can have a major impact on low- and middle-income countries.
A major roadblock in developing effective interventions for bacterial infections is a limited understanding of their biology. How do they spread and how do we block this? Why might one person be more susceptible to disease than another? What role do asymptomatic infections play in transmission, and why do asymptomatic cases exist in the first place?
Pathogen genomics has skyrocketed as a public health tool during the SARS-CoV-2 pandemic, and presents a good starting point for answering these questions. However I believe the integration of multiple technologies, disciplines and data types will be necessary to harness the full power of genomics. This approach can maximise the biological knowledge generated from samples contributed by clinical study participants.
In my current research this takes the form of working to integrate pathogen genome sequencing with epidemiological data and approaches to infer risk factors for transmission. In future I am interested in investigating the interaction between host, pathogen and microbiome genomics in disease, and in the use of multi-omics to identify mechanisms of protection.
Previous research
Evolution of Pandemic Cholera at its Global Source
Reviews
Transcriptomics in Human Challenge Models
Host restriction, pathogenesis and chronic carriage of typhoidal Salmonella
Genomic, clinical and immunity data join forces for public health
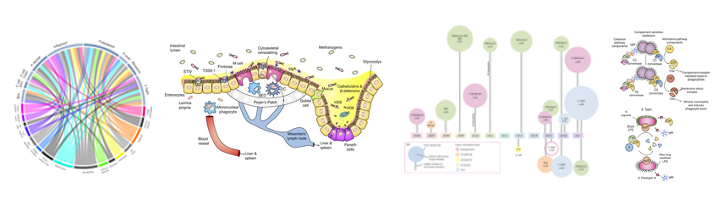
Host-pathogen interactions
Early transcriptional responses to human enteric fever challenge
Longitudinal Changes in Tear Cytokines and Antimicrobial Proteins in Trachomatous Disease
Investigation of the role of typhoid toxin in acute typhoid fever in a human challenge model

Immunogenetics
Genetic Susceptibility to Enteric Fever in Experimentally Challenged Human Volunteers
HLA-A, -B, -C, -DPB1, – DQB1 and -DRB1 allele frequencies of North Tanzanian Maasai
Sequence based HLA- DRB1, -DQB1 and -DPB1 allele and haplotype frequencies in The Gambia

