New research sheds light on cancer risk in gene therapies
Researchers from the Wellcome Sanger Institute, University of York and Boston Children’s Hospital analysed genetic changes in stem cells of a group of patients with sickle cell disease before and after they underwent gene therapy, finding an accumulation of stem cells with genetic mutations that affect blood cell growth.
The cause is likely not the gene therapy treatment itself, say researchers, but the therapy process, which involves gene editing outside the body and re-transplantation of stem cells back into the patient.
The findings, published today (16 November) in Nature Medicine, offer important new insights into processes happening in the body after gene therapy and may help inform safer treatments for sickle cell disease.
Sickle cell disease, an inherited genetic disorder, alters the natural round and flexible shape of red blood cells into a sickle or crescent shape, causing severe health issues and elevating the risk of blood cancer. Though around 100 million people carry the sickle cell trait worldwide1, the disease only occurs if a child inherits the trait from both parents. In regions where the trait is prevalent, such as parts of sub-Saharan Africa, up to 20 per cent of the population can be affected.
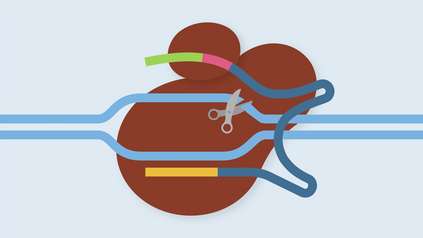
Recent advances in gene therapy offer hope for curing genetic conditions like sickle cell disease. Gene therapy involves modifying a sickle cell patient’s own stem cells outside the body, correcting the faulty gene responsible for the abnormal cell shape and re-introducing these into the patient.
In this new study, researchers set out to understand any cancer-related genetic changes for those who had undergone gene therapy.
Using a new approach, the team were able to track and compare blood cell samples from six patients with sickle cell disease before and after their treatment. They discovered that post-treatment there was an accumulation of stem cells carrying genetic mutations that impact the growth of blood cells. These mutations have been previously seen at higher levels in elderly individuals and those with certain blood cancers, such as leukaemia.
They found that the gene therapy treatment itself is not the likely cause of new DNA mutations in blood stem cells. Instead, the process of genetically modifying these stem cells outside the body and re-transplanting them back into the patient makes blood stem cells that already have these mutations more prominent, thereby increasing their influence on the blood and immune systems.
The researchers suggest that younger patients may have acquired fewer stem cell mutations in their lifetime, which may inform the optimal age for gene therapies in this and other diseases in the future.
While challenges remain in determining the long-term effects of such mutations, the work indicates some preventative measures to refine gene therapy treatment. It underscores the need for long-term monitoring of stem cell samples from patients with genetic conditions in order to track mutations that could lead to blood cancer.
“Think of the gene therapy process like clearing a forest and planting new seedlings. If you imagine that some seedlings are red and some are green, then the ‘selection’ we are observing is akin to having the forest regrow red trees preferentially.
“Our research indicates that gene therapy imposes a selection on different blood stem cells, the ‘seed’ cells of our blood and immune system. After gene therapy, the treatment might favour growth of stem cells with certain mutations, and this in turn could potentially lead to expansion of blood cells containing these mutations. In other settings, such expansions have been associated with development of blood cancers, particularly in older individuals, but the relationship of this study’s findings to the risk of blood cancers is not yet fully understood.”
Professor David Kent, senior author of the study, the Department of Biology and York Biomedical Research Institute
“Gene therapy holds immense potential to cure genetic conditions such as sickle cell disease, and understanding how the process influences blood stem cell growth in the long run is crucial for safety. Notably, our study revealed that younger patients, with fewer genetic mutations in their stem cells, didn’t exhibit strong signs of mutations post-therapy. This suggests that treating patients with gene therapy at a younger age could be both safer and more effective, but substantial work needs to be done to test this formally.”
Dr David Williams, senior author of the study,Boston Children’s Hospital and Harvard Medical School
“Our research revealed that both gene-therapy modified and unaltered stem cells from sickle cell patients sometimes contained cancer-associated mutations leading to accelerated growth through the gene therapy procedure. Continuously tracking these mutations and gaining a deeper understanding of these processes will profoundly impact the future well-being of sickle cell patients around the world.”
Dr Michael Spencer Chapman, author of the paper, Wellcome Sanger Institute
More information
1. https://www.afro.who.int/health-topics/sickle-cell-disease
Publication:
M. Spencer Chapman et al. Clonal selection of hematopoietic stem cells after gene therapy for sickle cell disease. (2023) Nature Medicine. DOI: 10.1038/s41591-023-02636-6