Could Genetics Improve Warfarin Dosing?
An international team of researchers have developed a way to use genetic information from patients that could help doctors better determine optimal doses of the common blood-thinning drug, warfarin. The results of the analysis – based on information from thousands of genetically and geographically diverse patients – are published in The New England Journal of Medicine.
In the large-scale study and an upcoming clinical trial, scientists supported by the US National Institutes of Health (NIH) address one of the trickiest issues in prescribing medicine: how to quickly optimize each patient’s dosage of warfarin.
One of the most widely prescribed drugs in the world, warfarin is used to prevent dangerous blood clots that can lead to heart attacks, strokes or even death. The drug is challenging for doctors to prescribe because the ideal dosage for each person varies widely and is hard to predict, yet is crucial for the patient’s safety.
In an important step toward putting the findings into clinical practice, NIH is launching the largest prospective, multi-centre, randomized clinical trial to test whether a gene-based strategy for prescribing the initial warfarin dose will improve patient outcomes. The trial will enrol 1,200 participants of diverse backgrounds and ethnicities at twelve clinical sites, and is scheduled to begin next month.
“In these investigations, NIH-funded basic research and clinical trials are working hand-in-hand to improve the care of the millions of patients on warfarin therapy. More broadly, these efforts showcase NIH’s firm commitment to building a future of personalized medicine: a future in which doctors will be able to prescribe the optimal dosage of medicine for each patient right from the start.”
Raynard S Kington MD, PhD, acting NIH director
Everyone responds differently to warfarin: one person may need 10 times more of the drug than another. Doctors typically select the initial dose based on standard clinical factors – such as age, weight and gender – then fine-tune the dosage over a few weeks in response to periodic tests of the blood’s ability to clot.
Researchers know that two genes, CYP2C9 and VKORC1, which vary slightly among individuals, can influence warfarin’s effectiveness. However, scientists do not know whether information about these genes can improve optimal dosage prediction for a wide range of patients, regardless of race, ethnicity or other genetic differences.
To investigate this issue, researchers across the globe joined together to form the International Warfarin Pharmacogenetics Consortium (IWPC). The patients they studied came from around the globe, including Taiwan, Japan, Korea, Singapore, Sweden, Israel, Brazil, the United Kingdom and the United States.
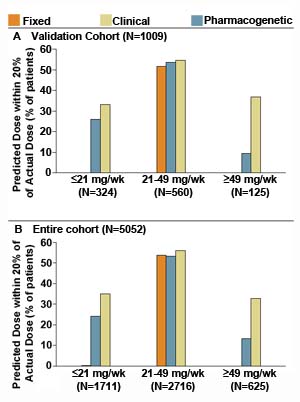
The results revealed that when genetic information was included, the predictions of ideal dosages were more accurate, especially for patients at the low or high ends of the dosing range. This is significant because nearly half of those on warfarin are at the extremes of the range, and these patients are typically at the greatest risk for excessive bleeding or clotting. By quickly optimizing dosages for these patients, doctors could minimize dangerous complications and improve the effectiveness and safety of warfarin treatment.
“By sharing information and expertise, the consortium researchers developed a way to dose warfarin that is based on data from patients around the world. This is a highly commendable example of international cooperation and data sharing and should increase the potential utility of the results.”
Jeremy M. Berg Ph.D., director of the National Institute of General Medical Sciences (NIGMS), which partially funded the study
Although doctors can now use US Food and Drug Administration-approved genetic tests to help determine the initial dose of warfarin, a large, randomized clinical trial – the gold standard for testing medical therapies – is needed to determine if the more precise, gene-based prescribing strategy is the best option.
“Warfarin genetics has been a major success story so far, few genetic studies of complex traits can claim having a model explaining over 40 per cent of the variance. But what counts in this instance is the strong potential such a simple genetic test has to improve patient healthcare.”
Panos Deloukas from the Wellcome Trust Sanger Institute
A new clinical trial To be conducted in the US, will provide important evidence to determine if genetic information gives added benefit for determining initial warfarin doses above and beyond what can be obtained with clinical information.
Researchers will assess how long participants in each group maintain the desired level of blood thinning, as determined by a blood test, at two and four weeks after starting therapy, as well as at three and six months. Researchers will also review bleeding problems and other complications, quality of life and cost of therapy.
“If the new clinical trial confirms the value of using a gene-based prescribing strategy for warfarin dosing, it will be a boon for patients and a major step toward the future of personalized medicine.”
Raynard Kington, NIH
More information
Participating Centres and Funding
A full list of participating centres and funding agencies is available at the New England Journal of Medicine website.
Publications:
Selected websites
The National Institutes of Health (NIH)
The National Institutes of Health (NIH) – The Nation’s Medical Research Agency – includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. It is the primary Federal agency for conducting and supporting basic, clinical and translational medical research, and it investigates the causes, treatments and cures for both common and rare diseases.
The Wellcome Trust Sanger Institute
The Wellcome Trust Sanger Institute, which receives the majority of its funding from the Wellcome Trust, was founded in 1992. The Institute is responsible for the completion of the sequence of approximately one-third of the human genome as well as genomes of model organisms and more than 90 pathogen genomes. In October 2006, new funding was awarded by the Wellcome Trust to exploit the wealth of genome data now available to answer important questions about health and disease.
The Wellcome Trust
The Wellcome Trust is a global charitable foundation dedicated to achieving extraordinary improvements in human and animal health. We support the brightest minds in biomedical research and the medical humanities. Our breadth of support includes public engagement, education and the application of research to improve health. We are independent of both political and commercial interests.


